When patients undergo a home sleep study to evaluate for sleep apnea or other sleep-related disorders, a negative result can sometimes leave them wondering what comes next. A negative test may provide reassurance for some, but for others—particularly those with persistent symptoms of disrupted sleep, daytime fatigue, or other related issues—it raises important questions about whether further testing or evaluation is warranted.
This article explores the next steps when a home sleep study is negative but clinical suspicion remains high.
What Is a Home Sleep Study?
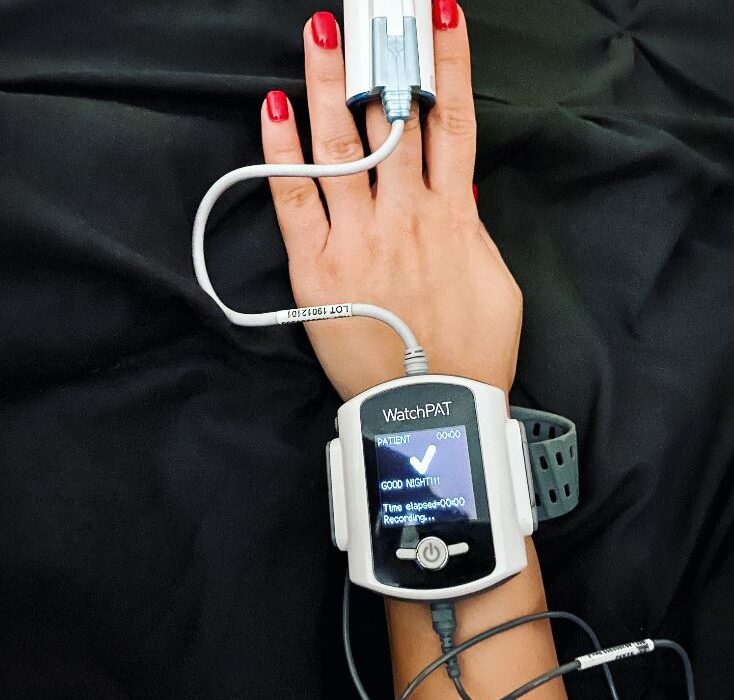
A home sleep study, also known as a home sleep apnea test (HSAT), is a simplified diagnostic tool designed to evaluate for obstructive sleep apnea (OSA) in the comfort of a patient’s home. These tests monitor key parameters such as:
- Respiratory effort
- Oxygen saturation
- Airflow
- Heart rate
Home sleep studies are generally cost-effective and convenient, making them an excellent first-line diagnostic tool for moderate-to-high-risk OSA in uncomplicated cases.
However, HSATs have limitations. They are less sensitive for mild OSA, central sleep apnea, and other sleep disorders such as periodic limb movement disorder, narcolepsy, or insomnia. False negatives may occur, especially if the equipment is not worn correctly, or if the disorder is less pronounced during the study night.
When a Negative Home Sleep Study Occurs
A negative result from a home sleep study means the test did not detect clinically significant sleep apnea. While this may be a valid outcome, several factors should be considered:
- Persistent Symptoms: If the patient continues to experience excessive daytime sleepiness, loud snoring, or witnessed apneas, the clinical suspicion for sleep-disordered breathing remains high.
- Risk Factors: Patients with obesity, hypertension, Type 2 diabetes, or craniofacial abnormalities are at higher risk for sleep apnea, even if a home test is negative.
- Comorbid Conditions: Certain conditions, such as chronic obstructive pulmonary disease (COPD) or congestive heart failure, may complicate the interpretation of home study results.
Next Step: In-Lab Polysomnography
For patients with persistent symptoms and high clinical suspicion despite a negative HSAT, the gold standard follow-up is an in-lab polysomnography (PSG). This comprehensive study provides a detailed analysis of sleep parameters and can diagnose a wide range of sleep disorders beyond obstructive sleep apnea.
During a PSG, the following are monitored:
- Brain activity (EEG): Identifies sleep stages and arousals.
- Eye movements (EOG): Assesses REM sleep.
- Muscle activity (EMG): Evaluates limb movements and atonia during REM sleep.
- Heart rate and rhythm (ECG): Detects arrhythmias.
- Respiratory effort and airflow: Differentiates central from obstructive apneas.
- Oxygen saturation: Detects desaturations due to hypoventilation or apneas.
Clinical Evidence Supporting PSG After a Negative HSAT
Research underscores the importance of in-lab testing when symptoms persist despite a negative home study:
- Sensitivity Issues with HSAT: Studies show that home sleep tests have lower sensitivity compared to PSG, particularly in mild cases or when comorbid sleep disorders are present. A 2020 meta-analysis found HSAT sensitivity to be approximately 79% compared to PSG for diagnosing OSA in moderate-to-severe cases. This leaves a significant margin for false negatives.
- Complex Sleep Apnea Syndromes: HSAT cannot reliably identify central sleep apnea, which often coexists with OSA in conditions such as heart failure or opioid use. A 2018 study in Chest highlighted the value of PSG in diagnosing complex sleep apnea syndromes missed by HSAT.
- Mild OSA: Home studies may fail to detect mild OSA, which can still significantly affect quality of life. In such cases, PSG offers greater diagnostic accuracy.
Other Considerations
Before proceeding with an in-lab study, the following should be evaluated:
- Proper HSAT Use: Review whether the patient followed instructions correctly and whether technical issues (e.g., dislodged sensors) may have impacted results.
- Alternative Diagnoses: Consider whether symptoms might be due to other disorders, such as restless legs syndrome, primary insomnia, or narcolepsy, which require specific testing or clinical evaluation.
Why It Matters
Identifying and treating sleep disorders is critical for overall health. Untreated sleep apnea, for instance, increases the risk of cardiovascular disease, stroke, diabetes, and motor vehicle accidents. A negative home sleep study should not be the end of the road if clinical suspicion remains high. The combination of clinical evaluation, patient history, and advanced diagnostics like PSG ensures no sleep disorder is overlooked.
Conclusion
When a home sleep study is negative but symptoms persist, an in-lab polysomnography is the logical next step. This comprehensive diagnostic tool not only confirms or rules out sleep apnea but also identifies other potential sleep disorders. By taking this step, patients can achieve an accurate diagnosis and begin appropriate treatment to improve their sleep and overall health.
If you’ve had a negative home sleep study and still experience sleep-related symptoms, consult your sleep specialist to discuss whether in-lab testing is right for you.
Clinical References
- Zou D, Grote L, Peker Y, Lindblad U, Hedner J. “Validation a home sleep apnea test against in-laboratory polysomnography in a population cohort.” Sleep Medicine. 2020.
- Javaheri S, Dempsey JA. “Central Sleep Apnea.” Chest. 2018; 153(3): 682-692.
- Kapur VK, Auckley DH, Chowdhuri S, et al. “Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline.” Journal of Clinical Sleep Medicine. 2017;13(3):479-504.